Why Understanding Scar Treatment Matters
Scar treatment encompasses a wide range of options designed to improve the appearance, texture, and function of scars after skin injury or surgery. Here’s what you need to know:
Quick Answer: Your Scar Treatment Options
- At-Home Care: Silicone gels/sheets, sunscreen (SPF 30+), massage, retinoids, vitamin C serums
- Injectable Treatments: Corticosteroid injections for raised scars, dermal fillers for depressed scars
- Surface Treatments: Chemical peels, microneedling, dermabrasion, laser therapy
- Surgical Options: Scar excision, Z-plasty, skin grafts for severe or restrictive scars
- Timeline: Most scars improve over 1-2 years; treatments work best on newer scars
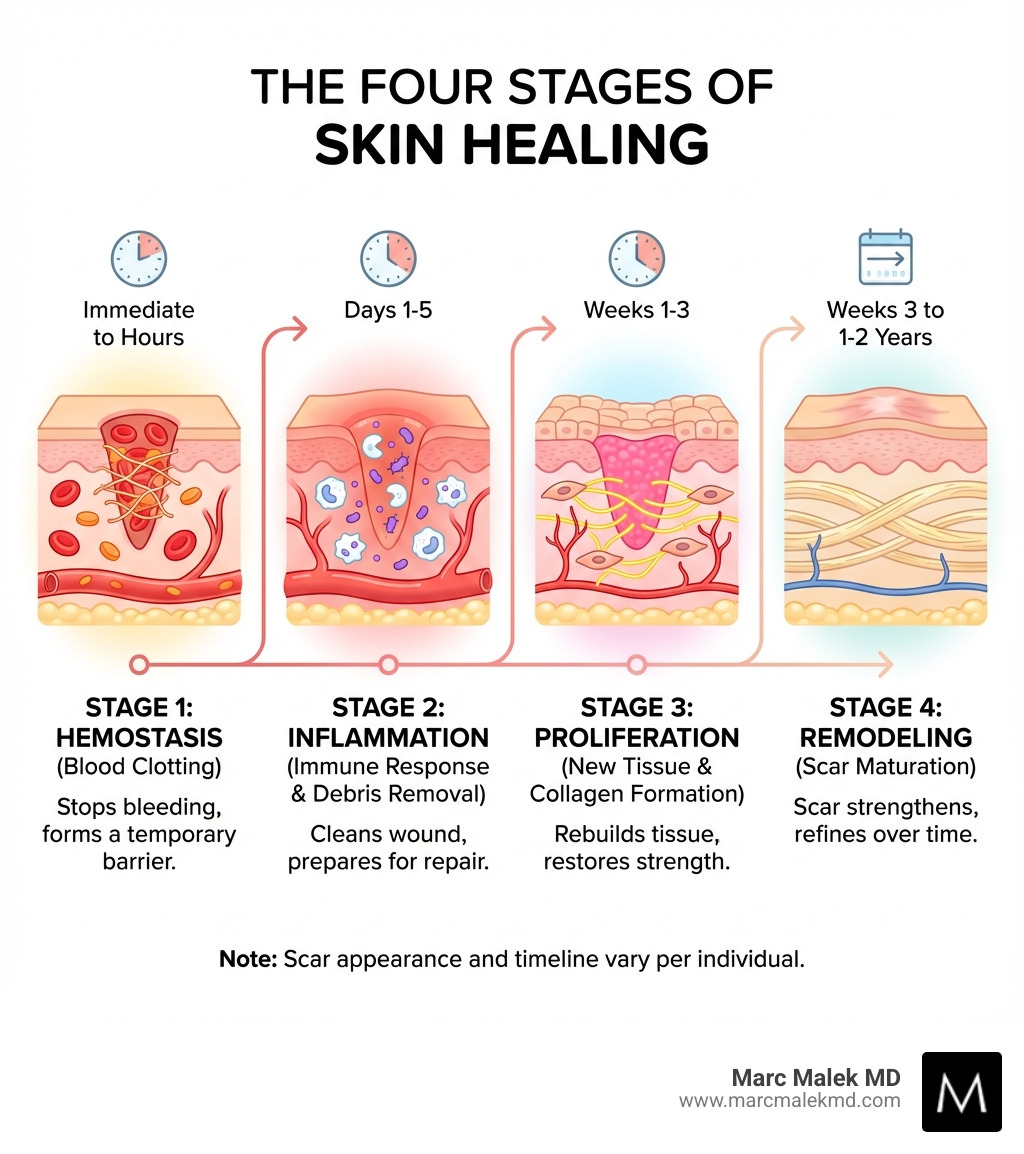
Scars are a natural part of your body’s healing process. When your skin repairs itself after injury, surgery, or conditions like acne, it forms scar tissue made primarily of collagen. While scars are permanent, their appearance can be dramatically improved with the right approach.
Nearly everyone develops some type of scar during their lifetime. These marks can result from accidents, surgical procedures, burns, acne, or illnesses like chickenpox. The way your scar forms depends on many factors—the depth and size of the wound, its location on your body, your age, genetics, and even your skin tone.
Most scars fade naturally over time, typically improving for up to two years after the initial injury. However, some scars remain visible, cause discomfort, restrict movement, or affect your confidence. That’s where modern scar treatment comes in.
The good news? Studies show that advanced treatments can reduce scar size by 50% or more. In some cases, scars can become so faint they’re barely noticeable. Whether you’re dealing with surgical scars, acne marks, or keloid formations, a combination of proper wound care, at-home management, and professional treatments can help you achieve smoother, more confident skin.
Understanding Your Scar: Types and Characteristics
Scars are your body’s way of telling a story—a story of healing after an injury, surgery, or even a pesky pimple. But not all scars are created equal, and understanding their differences is the first step toward effective scar treatment. While scars are fibrous tissue that replaces lost or damaged skin, their appearance, texture, and behavior can vary widely. Factors like the severity of the injury, its location on the body, your age, genetics, and even your nutritional status can influence how a scar looks and heals.
It’s also important to distinguish between a true scar and simple color changes on the skin. Residual discoloration, such as post-inflammatory hyperpigmentation (PIH) which causes dark spots, or post-inflammatory erythema (PIE) which results in red or pink marks, are not scars. These color changes are typically easier to treat and often fade over time, unlike true scars that involve textural changes to the skin and are permanent.
Let’s explore the main types of scars we encounter:
Atrophic (Depressed) Scars
Atrophic scars are characterized by their sunken or pitted appearance. They form when there’s a loss of tissue, specifically collagen, during the healing process. This deficiency prevents the skin from fully regenerating to its original level, leading to an indentation.
- Acne Scars: These are perhaps the most common type of atrophic scars. They can manifest in various forms:
- Ice pick scars: Small, narrow, deep holes that look like the skin has been punctured by an ice pick.
- Boxcar scars: Wider, U-shaped scars with sharp, defined edges, resembling chickenpox scars.
- Rolling scars: Broad depressions with sloping edges, giving the skin a wavy, uneven texture.
- Chickenpox Scars: Similar to boxcar acne scars, these are typically round or oval depressions left after the chickenpox lesions heal.
- Collagen Loss: The underlying cause for all atrophic scars is an insufficient production of collagen during the repair phase. As Dr. Robyn Gmyrek notes, “Atrophic scars, also known as depressed scars, are indented on the surface of the skin… caused by loss of collagen during the healing process.”
Hypertrophic and Keloid (Raised) Scars
These scars are characterized by an overproduction of collagen, leading to a raised texture. They can often be red, itchy, or even painful. While they share similarities, their key difference lies in their growth pattern.
- Hypertrophic Scars: These are raised, red, and thickened scars that remain confined to the original wound’s boundaries. They typically develop within weeks of an injury and may improve naturally over a year or more.
- Keloid Scars: Unlike hypertrophic scars, keloids grow aggressively beyond the borders of the original injury, forming thick, rounded, irregular clusters of scar tissue. They can appear pink, red, or flesh-toned and are often hairless. Keloids can develop up to a year after the initial trauma and are more common in individuals with darker skin tones and those with a genetic predisposition. As Dr. Zakia Rahman explains, “keloid scars grow beyond the borders of the original injury.” Keloids are notoriously difficult to treat because they are unpredictable and have a high recurrence rate, even after treatment, as highlighted by Dr. Mara Weinstein Velez. Scientific research on keloid scars emphasizes their complex nature and challenges in management.
Contracture Scars
Contracture scars occur when a large area of skin is damaged and lost, leading to scar tissue that pulls the skin edges together. This creates a tight area that can significantly restrict movement, particularly if the scar is near a joint or affects muscles and tendons.
- Burn Injuries: These are a common cause of contracture scars, as significant burns often result in extensive skin damage.
- Skin Tightening and Restricted Movement: The scar tissue contracts, pulling on the surrounding skin and deeper tissues, which can lead to a decrease in the affected body part’s range of motion. Treating contractures often requires surgical intervention to release the tightened tissue and restore function.
Initial Wound Care and At-Home Scar Management
The journey to minimizing visible scarring begins the moment an injury occurs. Proper initial wound care is paramount and can significantly influence the final appearance of a scar. Think of it as laying the groundwork for smoother skin!
First Steps for Minimizing Scar Formation:
- Cleanliness is Key: Gently clean the wound with mild soap and water. This helps prevent infection, which can worsen scarring.
- Keep it Moist: Applying an antibacterial ointment or petroleum jelly (like Vaseline) keeps the wound moist. This creates a protective barrier, facilitates the healing process, and minimizes scab formation. Scabs actually hinder optimal healing and can lead to more noticeable scars.
- Cover Up: Use a non-stick bandage or dressing to protect the wound from dirt, bacteria, and physical trauma. Change bandages daily to maintain cleanliness.
- Avoid Picking: Resist the urge to pick at scabs or manipulate the healing skin. This can disrupt the delicate new tissue and lead to increased inflammation and scarring.
- Sun Protection: This is crucial! Protect healing scars from sun exposure, especially for the first year. UV rays can cause scars to darken and become more noticeable (hyperpigmentation). Use clothing, dressings, or a broad-spectrum sunscreen with SPF 30 or higher.
- Minimize Tension: For new wounds, especially surgical incisions, minimizing tension on the healing edges can prevent widening of the scar. This is where products like silicone sheets or even special surgical tapes can play a role.
- Nutrition: Support your body’s healing with good nutrition, including adequate protein and vitamins C and D, which are essential for collagen production and overall skin health.
Best Practices for At-Home Scar Treatment
Once the wound has closed and is no longer open, you can begin more targeted at-home scar treatment strategies. Consistency is vital, as these treatments often take several weeks or even months of continuous use to show improvement.
- Silicone Gels and Sheets: These are considered the gold standard for topical scar management and have the best evidence for reducing scar appearance. As Dr. Joshua Zeichner states, “After the wound closes, silicone gels can help the scar heal the best it can.” Silicone works by hydrating the skin, regulating collagen production, and protecting the scar from the environment. Sheets should be worn for more than 12 hours a day, often for months, while gels offer a more discreet option. We recommend products like Kelo-Cote Advanced Formula Scar Gel or ScarAway Clear Silicone Scar Sheets.
- Petroleum Jelly (Vaseline): Even after initial healing, continuing to massage ointments like Vaseline onto the scar can help soften scar tissue. It creates a protective barrier and keeps the area moist, aiding in the remodeling phase.
- Scar Massage Techniques: Once the wound is fully closed, gentle massage with a water-based cream (like aqueous cream or E45 cream) can improve scar pliability and reduce stiffness. Massaging for 5-10 minutes a few times a day can be beneficial.
- Retinoids: Both over-the-counter retinol and prescription-strength retinoids can be effective for improving uneven skin tone and texture, particularly for post-acne dark spots and some atrophic scars. They work by increasing skin cell turnover and stimulating collagen. However, they are not effective for raised scars and can cause irritation, so use with caution and under guidance.
- Vitamin C Serums: As a powerful antioxidant, Vitamin C can help reduce redness and mild color changes associated with scars, promoting a brighter complexion. It doesn’t, however, address scar thickness or texture directly.
- Onion Extract Creams: While popular, research on the effectiveness of onion extract (e.g., in Mederma Advanced Scar Gel) is mixed. Some find it helpful for mild improvements in scar appearance, but it’s generally less effective than silicone for raised scars.
Here’s a list of common ingredients found in over-the-counter scar treatments:
- Silicone: (Gels, sheets, liquids) Creates a protective barrier, hydrates, and regulates collagen.
- Onion Extract (Allium Cepa): Believed to reduce inflammation and collagen production, but evidence is variable.
- Allantoin: Moisturizes and helps shed dead skin cells.
- Vitamins C and E: Antioxidants, can help with discoloration and skin health. Vitamin E’s scar-improving effects are not strongly supported by evidence, and it can sometimes cause irritation.
- Hyaluronic Acid: Hydrates and plumps the skin.
- Peptides: Can support collagen production and skin repair.
- Hydroquinone: (Often prescription) A skin-lightening agent for hyperpigmentation, not for scar texture.
- Alpha Hydroxy Acids (AHAs) / Beta Hydroxy Acids (BHAs): Chemical exfoliants that can improve surface texture and discoloration.
- Tranexamic Acid, Kojic Acid, Azelaic Acid, Niacinamide: Ingredients targeting discoloration and hyperpigmentation.
Professional Scar Treatment Options
While at-home care can significantly improve scar appearance, some scars require professional intervention to achieve optimal results. This is where the expertise of a board-certified plastic surgeon or dermatologist in Scottsdale, Phoenix, or throughout Arizona becomes invaluable. They can accurately diagnose your scar type, assess its characteristics, and recommend a personalized scar treatment plan, often involving combination therapies. Our goal is always to deliver fantastic, long-lasting results, focusing on your comfort and promoting a healthy lifestyle.
Injections and Fillers
Injectable treatments offer targeted solutions for specific scar types, working beneath the skin’s surface.
- Corticosteroid Injections: These are a cornerstone treatment for raised, thick, or red scars, including hypertrophic scars and keloids. Injected directly into the scar, corticosteroids reduce inflammation, flatten the scar, and alleviate symptoms like itching and pain. Treatments are typically given at 4-6 week intervals for several months. Studies show these injections can reduce scar size by 50% or more, sometimes making the scar appear almost gone.
- 5-FU or Bleomycin Injections: These chemotherapy drugs can also be injected into raised scars, particularly keloids, to flatten them and ease symptoms. They work by inhibiting fibroblast proliferation.
- Dermal Fillers for Atrophic Scars: For depressed or pitted scars (like certain acne scars), dermal fillers (such as hyaluronic acid-based products or collagen stimulators) can be injected to raise the indentation to the level of the surrounding skin. This adds volume, creating a smoother appearance.
Surface and Light-Based Therapies
These treatments work on the outer layers of the skin to improve texture, color, and overall appearance.
- Chemical Peels: Chemical peels involve applying a chemical solution to the skin, which exfoliates the top layers. Light peels can improve discoloration and superficial texture, while medium to deep peels can address more significant textural changes and sun damage. Different types of peels are used for acne scars, sun damage, wrinkles, and melasma.
- Dermabrasion: This procedure involves using a rapidly rotating brush or device to “sand” away the top layers of skin. It’s effective for smoothing skin lines, improving the appearance of acne scars, and reducing age spots and sun damage. As the skin heals, new, smoother skin replaces the treated area.
- Microneedling: This technique uses a device with fine needles to create controlled micro-injuries in the skin. These tiny punctures stimulate the body’s natural collagen and elastin production, which helps to remodel scar tissue and improve texture, particularly for atrophic scars. Microneedling can also be combined with radiofrequency (like Morpheus8) for improved scar smoothing and collagen stimulation.
- Laser Therapy: Laser technology has revolutionized scar treatment, offering precise and effective solutions for a wide range of scar concerns. Our practice in Scottsdale specializes in advanced laser treatments, including CO2 laser resurfacing. Lasers work by delivering targeted energy to the scar tissue, stimulating collagen remodeling, reducing redness, and improving texture.
- Pulsed-Dye Lasers (PDL): Often used for red or vascular scars, PDLs target blood vessels to reduce redness and flatten raised scars. Studies have shown significant improvement in hypertrophic scars and keloids with PDL treatment.
- Fractional CO2 Lasers: These lasers create microscopic columns of injury in the skin, leaving surrounding tissue intact. This stimulates intense collagen production and remodeling, making them highly effective for improving the texture of atrophic scars (e.g., acne scars) and surgical scars. They can also flatten and soften raised scars. More info about laser technology and Erase Scars with the Help of Laser Technology provide further details on how these advanced techniques work. For a deeper dive into the science, an Expert overview of laser scar revision explains the mechanisms and various modalities.
Surgical Scar Treatment and Revision
When scars are severe, cause significant functional impairment, or are unresponsive to less invasive methods, surgical scar treatment and revision may be recommended. Our team in Scottsdale, Phoenix, and Arizona is adept at utilizing a personal and artistic approach to scar revision, ensuring the best possible aesthetic and functional outcomes.
- When Surgery is Recommended: Surgery is typically considered for scars that:
- Are very large or disfiguring.
- Restrict movement (contractures).
- Are deeply depressed or significantly raised.
- Are located in prominent areas and cause self-consciousness.
- Scar Excision: This involves surgically removing the existing scar and carefully re-closing the wound to create a new, less noticeable scar. This is often done with meticulous suturing techniques to minimize tension and optimize healing.
- Z-Plasty or W-Plasty: These specialized surgical techniques are used to reposition or break up linear scars. They involve creating small, geometric flaps of skin that are rearranged to alter the scar’s direction, often placing it into a natural skin crease or fold, making it less conspicuous. Z-plasty is also used to release tension in contracture scars, improving flexibility.
- Skin Grafts and Flaps: For very large or deep scars, especially those resulting from burns or extensive trauma, skin grafts or flaps may be necessary.
- Skin Grafts: Healthy skin is taken from another part of your body (donor site) and transplanted to cover the scarred area.
- Skin Flaps: Similar to grafts, but a flap includes not just skin but also underlying tissue (fat, muscle) and its own blood supply. This is used when the recipient area has poor circulation or requires more robust tissue.
- Tissue Expansion: This technique involves inserting a balloon-like device (tissue expander) under healthy skin adjacent to the scar. Over several weeks, the expander is gradually filled with saline, stretching the skin. Once sufficient new skin is created, the expander is removed, and the stretched skin is used to replace the scar, often providing a better color and texture match than a graft from a distant site. This is frequently used in conjunction with flap surgery for contractures.
Frequently Asked Questions about Scar Treatment
We understand that dealing with scars can bring up many questions. Here, we address some of the most common inquiries our patients have about scar treatment.
How long does it take for a scar to improve?
The improvement of a scar is a journey, not a sprint. Scar formation is a natural process, and the skin undergoes new tissue formation and remodeling, incorporating collagen to help with scar formation. Here’s a general timeline:
- Initial Healing Phase: This is the first few weeks after the injury. The wound closes, and new skin begins to form. During this time, the scar may appear red or pink and slightly raised.
- Maturation Phase: This phase can last anywhere from six months to two years, or even longer. During this time, the scar tissue remodels, collagen fibers reorganize, and blood vessels diminish. The scar typically softens, flattens, and fades in color. Most scars will improve and fade over a period of up to two years. After this time, it is unlikely they will continue to fade significantly on their own.
- Factors Affecting Timeline: The duration and degree of improvement depend on several factors, including:
- Age: Younger skin tends to heal more vigorously, sometimes leading to more pronounced scars.
- Location: Scars on areas with more movement or tension (like joints or the chest) may take longer to mature or be more noticeable.
- Scar Type: Keloids and hypertrophic scars, due to their excessive collagen production, take longer to flatten and fade, if they do so naturally at all.
- Individual Healing: Everyone’s body heals differently, influenced by genetics, skin type, and overall health.
- When to Expect Results from Treatments: While natural fading takes time, professional treatments can accelerate this process.
- Topical OTC treatments: Can take several weeks or months of continuous treatment to show improvement.
- Injections: Effects can be seen after a few sessions (e.g., corticosteroids over several months).
- Laser or surface treatments: Can show impressive results over a series of sessions, often making scars look significantly better within months.
Can old scars be treated effectively?
Yes, old scars can absolutely be treated effectively, though the approach might differ from treating new scars. It’s a common misconception that once a scar is “old,” nothing can be done. While older scars are generally harder to treat than newer ones, significant improvement is still possible.
- Challenges of Treating Old Scars: Mature scars have already completed their remodeling phase, meaning the collagen structure is more stable and less amenable to natural changes. They might be firmly set in terms of texture, color, and depth.
- Available Treatments for Mature Scars: Many of the professional treatments we discussed, such as laser resurfacing, microneedling, chemical peels, dermal fillers, and surgical revision, are highly effective for older scars. For example, laser therapy can help remodel old collagen and improve both texture and discoloration.
- Improvement vs. Removal: While treatments can dramatically improve the appearance of an old scar—making it smoother, flatter, less red, or less noticeable—no treatment can completely erase a scar. Our goal is always significant improvement.
- Importance of Professional Consultation: Consulting with a board-certified plastic surgeon or dermatologist is crucial for old scars. They can assess the scar’s characteristics and recommend the most appropriate and effective treatment plan, which might involve a combination of therapies.
What is the most effective treatment for acne scars?
Acne scars are a very common concern, and thankfully, we have a wide array of effective scar treatment options available. The “most effective” treatment often depends on the specific type of acne scar you have and often involves a combination approach.
- Types of Acne Scars: As mentioned earlier, acne scars typically fall into the atrophic category, including:
- Ice Pick Scars: Deep, narrow, V-shaped pits.
- Boxcar Scars: Wider, U-shaped depressions with sharp edges.
- Rolling Scars: Broad, wave-like depressions.
- Combination Approach: For optimal results, we often recommend a multi-modal approach, combining different treatments to address various aspects of the scars.
- Key Treatments for Acne Scars:
- Laser Resurfacing: Fractional CO2 lasers are highly effective for improving the texture and depth of most atrophic acne scars. They work by stimulating collagen production and remodeling the skin. Studies show impressive results with laser therapy.
- Microneedling: This treatment, especially when combined with radiofrequency (like Morpheus8), is excellent for stimulating collagen and improving the overall texture and appearance of rolling and boxcar scars.
- Chemical Peels: Medium to deep chemical peels can improve the appearance of shallow boxcar and rolling scars, as well as address pigmentation issues.
- Dermal Fillers: For rolling and some boxcar scars, fillers can be injected beneath the scar to raise the depressed area, providing immediate smoothing.
- Subcision: This technique involves using a needle to break up the fibrous bands that pull rolling scars down, allowing the skin to rise.
- TCA CROSS: For ice pick scars, the CROSS (Chemical Reconstruction of Skin Scars) technique uses a high concentration of trichloroacetic acid (TCA) applied directly into the scar to stimulate collagen.
Your Path to Smoother Skin
Navigating scar treatment can feel overwhelming, but remember, you don’t have to face it alone. From the moment an injury occurs to the long-term management of mature scars, a spectrum of options exists to help you achieve smoother, more confident skin. We’ve explored everything from initial wound care and at-home remedies like silicone gels and retinoids, to professional interventions including corticosteroid injections, advanced laser therapies, and surgical revisions.
The key takeaway is the importance of a personalized plan. What works for one scar might not be ideal for another, and the best results often come from a combination of treatments custom to your specific scar type, skin characteristics, and aesthetic goals.
Several factors influence scar healing and appearance:
- Genetics: Your genetic makeup plays a significant role in how your skin heals, with some individuals being more prone to keloids or hypertrophic scars.
- Skin Type: Skin tone can influence the risk of hyperpigmentation (darkening) or hypopigmentation (lightening) in scars.
- Age: Younger skin, while regenerating quickly, can sometimes produce more robust scars.
- Injury Characteristics: The depth, size, location, and cause of the injury (e.g., surgical incision vs. burn) all impact the final scar.
When should you consult a plastic surgeon or dermatologist for scar treatment? We encourage you to seek professional advice if:
- Your scar is painful, itchy, or causes discomfort.
- It restricts your movement or affects function.
- You are unhappy with its cosmetic appearance.
- You notice any changes in the scar’s color, size, or texture.
- You are considering any cosmetic procedure and have a history of problematic scarring.
As Dr. Marc Malek, we approach every patient with a personal and artistic perspective, believing that by understanding your unique needs, we can deliver fantastic, long-lasting results. Our practice in Scottsdale, Phoenix, and Arizona is dedicated to patient comfort and convenience, promoting a healthy lifestyle alongside achieving proportionally balanced bodies.
While scars are a permanent reminder of your body’s incredible ability to heal, significant improvement is always within reach. Let us help you explore the possibilities and guide you on your path to smoother, more confident skin. Explore advanced Laser Skin Resurfacing options or consult a board-certified plastic surgeon to begin your personalized scar treatment journey.